Have you ever wondered how your body keeps itself in check—how it gets rid of cells that are damaged, unnecessary, or potentially dangerous? Enter apoptosis, often dubbed "programmed cell death." It’s a tightly controlled process that acts like a cellular self-destruct button, ensuring our tissues stay healthy and balanced. In this blog, we’ll dive into what apoptosis does, the key genes that run the show, the diseases tied to it when things go wrong, and what the future might hold for harnessing this pathway in medicine.
1. What Role Does Apoptosis Play in Cells?
Apoptosis is the body’s way of saying, “Thanks for your service, but it’s time to go.” It’s a natural process that eliminates cells we don’t need anymore—like the webbing between our fingers during fetal development—or cells that could harm us, like those with damaged DNA. Think of it as a quality control mechanism: it keeps our tissues functioning properly by maintaining the right number of cells and removing ones that are past their prime.
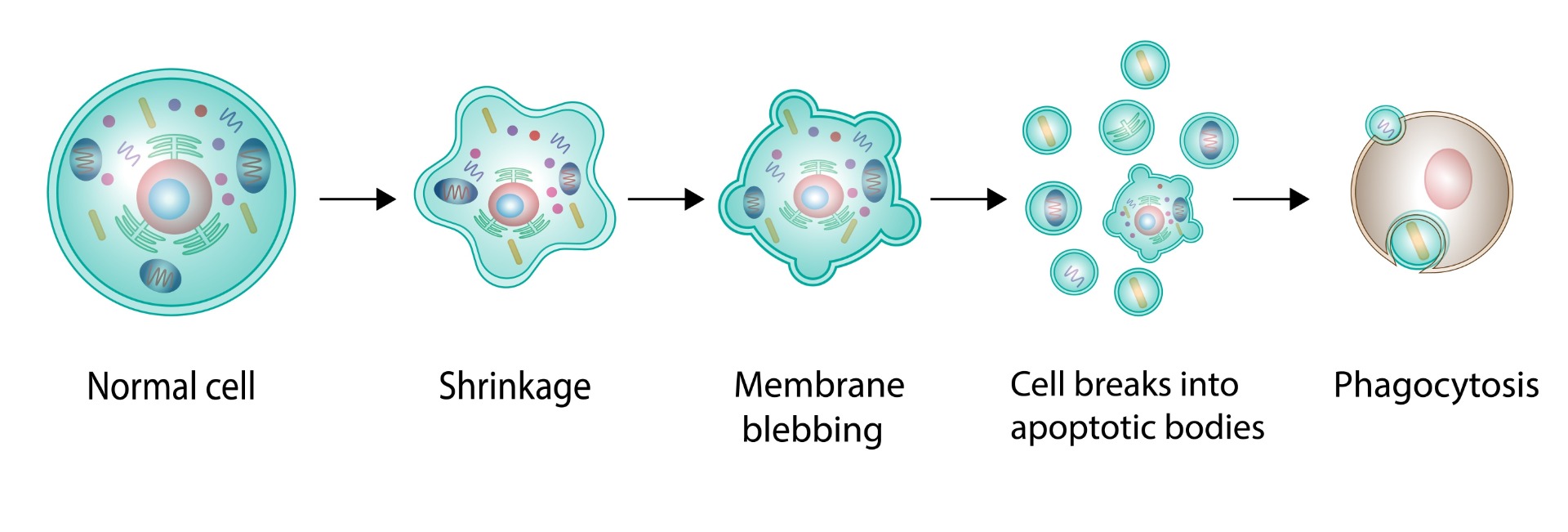
Unlike chaotic cell death (necrosis), which is messy and triggers inflammation, apoptosis is orderly. The cell shrinks, chops up its DNA, and breaks into small pieces called apoptotic bodies, which are quietly cleaned up by neighboring cells or immune cells. This process is crucial for development, immune system function, and preventing rogue cells from multiplying uncontrollably.
2. Major Genes Involved and Their Functions
Apoptosis is orchestrated by a cast of molecular players—genes and proteins that work together like a well-rehearsed theater troupe. Here are some of the stars:
-
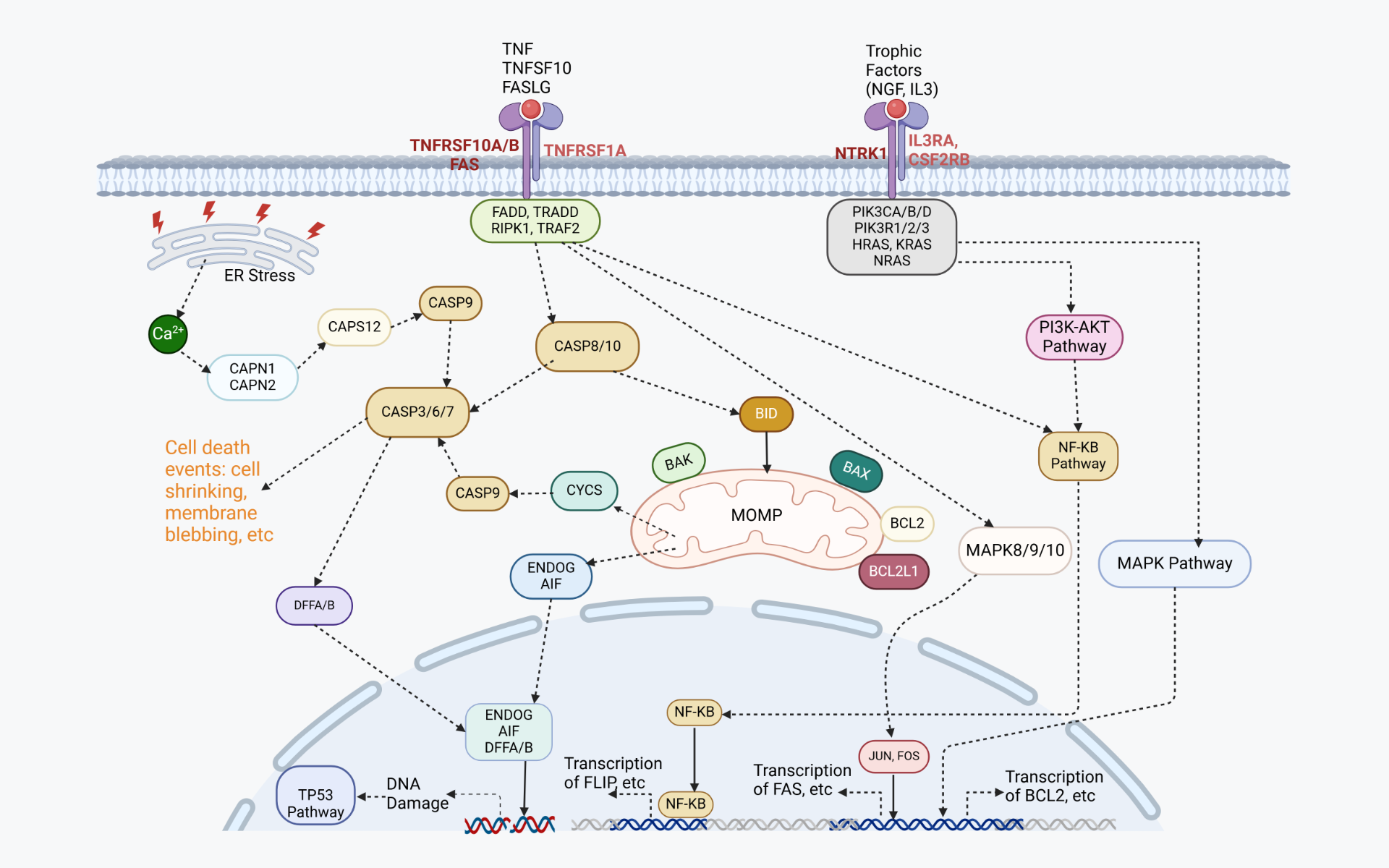
This group is the gatekeeper of apoptosis. It includes pro-apoptotic members like BAX and BAK, which poke holes in the mitochondria to release cell-death signals, and anti-apoptotic members like BCL-2 itself, which block these signals to keep cells alive. The balance between these two factions decides a cell’s fate.
-
Caspases: These are the executioners. Caspases like CASP3, CASP8, and CASP9 are enzymes that, once activated, dismantle the cell from the inside—cutting up proteins, fragmenting DNA, and ensuring a clean exit. They’re triggered by two main pathways: the intrinsic (mitochondrial) pathway, often sparked by internal stress, and the extrinsic (death receptor) pathway, triggered by external signals.
-
TP53 (p53): Known as the “guardian of the genome,” p53 senses DNA damage and can push a cell toward apoptosis if the damage is irreparable. It’s like a referee calling the game when things get too risky.
-
FAS and TNFR: These death receptors on the cell surface kick off the extrinsic pathway when they bind to specific ligands (like FAS ligand or TNF). They signal the caspases to get to work, no mitochondria required.
Each of these genes and proteins plays a specific role, ensuring apoptosis happens only when it’s supposed to—and stops when it’s not.
3. Diseases Linked to the Apoptosis Pathway
When apoptosis goes off-script, trouble brews. Too much or too little cell death can lead to serious health issues:
-
Cancer: If apoptosis fails (say, BCL-2 is overexpressed or p53 is mutated), damaged cells don’t die—they multiply. This is a hallmark of many cancers, allowing tumors to grow unchecked.
-
Neurodegenerative Diseases: Too much apoptosis can be just as bad. In diseases like Alzheimer’s, Parkinson’s, and Huntington’s, excessive cell death wipes out neurons, leading to progressive brain damage.
-
Autoimmune Disorders: Faulty apoptosis can prevent the elimination of self-reactive immune cells, contributing to conditions like lupus or rheumatoid arthritis, where the immune system attacks the body.
-
Viral Infections: Some viruses, like HIV, exploit apoptosis to kill off immune cells, while others block it to keep infected cells alive and churning out more virus.
The apoptosis pathway is a double-edged sword—its precision is vital, and any misstep can tip the scales toward disease.
4. Future Medical Applications
So, what’s next for apoptosis? Scientists are buzzing with ideas to tweak this pathway for medical breakthroughs:
-
Cancer Therapies: Drugs that kick apoptosis into gear—like BH3 mimetics (which mimic pro-apoptotic BCL-2 proteins)—are already in trials to force cancer cells to self-destruct. Imagine a treatment that flips the switch back on in cells that refuse to die!
-
Neuroprotection: On the flip side, blocking excessive apoptosis could save neurons in diseases like Alzheimer’s. Inhibitors targeting caspases or BCL-2 pathways might slow neurodegeneration.
-
Regenerative Medicine: Fine-tuning apoptosis could help in tissue engineering—clearing out old cells to make room for new, healthy ones grown from stem cells.
-
Viral Defense: Boosting apoptosis in infected cells or blocking viral tricks that inhibit it could be a new frontier in fighting infections.
The potential is huge, but the challenge lies in precision—targeting the right cells at the right time without collateral damage. As research unfolds, apoptosis could become a cornerstone of personalized medicine.
Wrapping Up
Apoptosis is more than just cell death—it’s a fundamental process that shapes life from the womb to old age. With genes like BCL-2, caspases, and p53 pulling the strings, it’s a marvel of biological engineering. When it misfires, diseases like cancer or neurodegeneration can take hold, but the future holds promise: by mastering this pathway, we might unlock treatments that save lives or improve their quality. Next time you marvel at your body’s resilience, give a nod to apoptosis—the unsung hero keeping it all in balance.
References
Carneiro, B. A., & El-Deiry, W. S. (2020). Targeting apoptosis in cancer therapy. Nat Rev Clin Oncol, 17(7): 395–417.
ELMORE, S. (2007). Apoptosis: A Review of Programmed Cell Death. Toxicologic Pathology, 35:495–516.
Fulda, S. (2011). Targeting apoptosis signaling pathways for anticancer therapy. Frontiers in Oncology, 1(23):1-7.
Green, D. R. ( 2022). The Mitochondrial Pathway of Apoptosis Part I: MOMP and Beyond. Cold Spring Harb Perspect Biol, 14:a041038.
Newton, K., Strasser, A., Kay, N., & Dixit, V. M. (2024). Cell death. Cell, 187:235-256.
Wong, R. S. (2011). Apoptosis in cancer: from pathogenesis to treatment. Journal of Experimental & Clinical Cancer Research, 30:87.